Overview
Chronic kidney disease is the most commonly diagnosed metabolic condition in senior cats affecting up to 80% of the older cat population. It is also quite commonly diagnosed on older dogs. Unlike in acute (sudden) kidney failure, the changes to the kidneys happen gradually, and often by the time the diagnosis has been made, the changes to the kidneys are irreversible. However, there are several interventions that can be implemented to potentially slow progression of kidney disease. We can also utilize certain treatments to keep our pets more comfortable and with an overall better quality of life if we catch the disease early. This is why routine screening for this disease is so highly recommended by veterinarians amongst our geriatric patients. While there is still a lot to be learned about kidney disease, we can review what is known about the disease process, diagnosis, risk factors, causes and potential treatment options for chronic kidney disease.
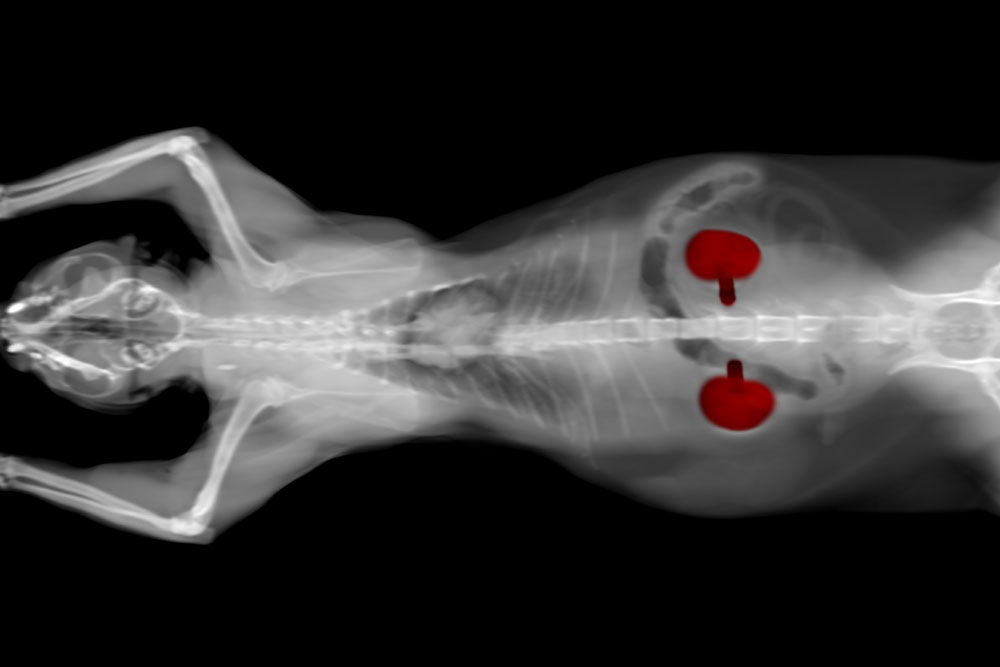
What Do Kidney’s Do
The primary job of the kidneys is to clear potentially harmful waste products from the blood stream. These waste products are often formed during the typical break down and utilization of food products to create energy. However, what is equally as important as removing the waste, is how the kidneys are able to retain other critical components of the blood such as protein, electrolytes, minerals, water, etc to keep a constant perfect balance within the body. The way in which they accomplish this is fairly complex, but here are the basics.
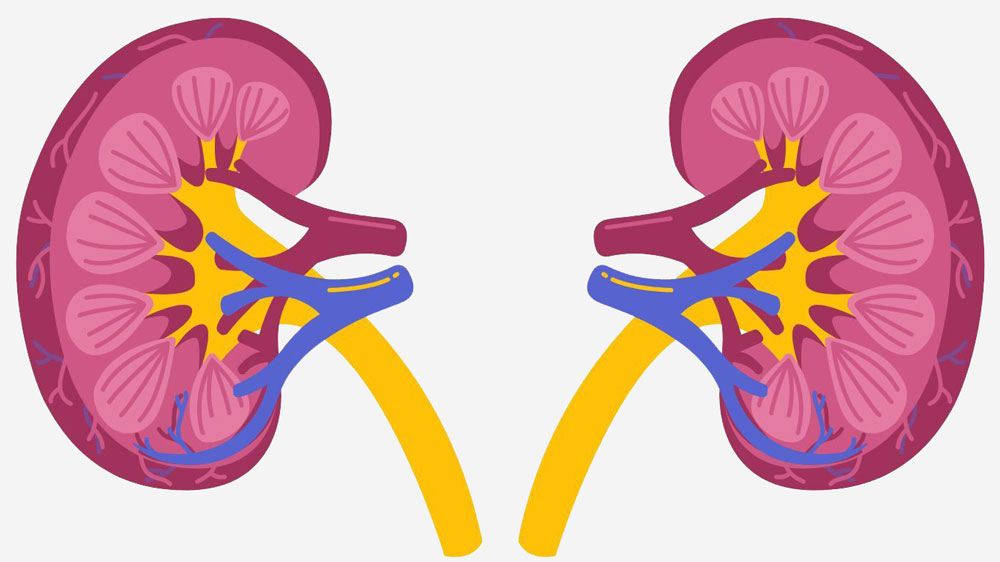
The kidney is composed of hundreds of thousands of units called nephrons. Each nephron is then further broken down into the glomerulus which acts like a tiny filter and the tubule, which is a transport tunnel on the other side of the filter. As blood is pumped through small vessels within the kidneys, the blood pressure causes various substances like electrolytes, sugars, water and waste products to pass through the filter (glomerulus) into the tubules. As the fluid moves through the tubule, the kidneys reclaim the water and other substances the body needs. In general, about 99% of the fluid that is filtered is reclaimed and the remaining 1% makes its way out of the tubules. As these tubules come together they form a collection reservoir of urine in the kidney, which flows through the ureters, into the bladder, and eventually out of the body.
In addition to the primary roles of excreting waste and retaining essentials the kidney has a few other roles, which it may share to some extent with other organs or glands. We consider these more like “side hustles” if you will, but can still be fairly important if overlooked for too long. These include:
- Making a hormone called erythropoietin, which stimulates to production of red blood cells.
- Modifying Vitamin D from its original form to its usable form called calcitriol.
- Providing a feed-back system for regulating blood pressure.
Signs of Kidney Disease
Depending on how advanced the disease is and the changes occurring in the kidneys, the signs of kidney disease can be quite variable. Because dogs and cats cannot tell us how they feel, most often the very subtle signs are missed and the disease is only caught in more advanced stages. This is particularly true of cats who are masters at hiding illness. These are some of the most common signs noted.
- Increased thirst and urination
- Build-up of waste products in the blood stream
- Lethargy
- Loss of appetite
- Weight loss
- Unkempt hair coat
- Nausea and Vomiting
- Constipation
- Blindness

Diagnosis and Staging of Kidney Disease
The diagnosis of kidney disease is usually based on certain changes noted in the pet’s bloodwork. These changes occur when the filtration ability of the kidneys declines so severely that waste products begin to build up in the blood stream. The two waste products most commonly screened for are urea nitrogen (BUN) and Creatinine (CREAT). Unfortunately, once these waste products can be detected in the blood stream the kidneys have already lost about 75% of their function. There is a newer test run by some laboratories called a symmetric dimethylarginine (SDMA) test that may detect kidney disease much earlier, when only 40% of the function has been lost. Of course, these changes must be considered in light of urine concentration, the pet’s history and exam findings before making the final diagnosis of chronic kidney disease. Sometimes more than one blood test is needed to confirm.
As you can imagine, diagnosing kidney disease when almost 75% of the function has been lost presents a bit of a challenge. The new SDMA test offers veterinarians a huge advantage in managing kidney disease at a much earlier stage. This is a big reason why routine blood screening every 6 months to 1 year is so strongly recommended. It allows us to look for trends in increasing BUN, CREAT and SDMA even before these values become abnormal to help predict kidney disease.

Once kidney disease is diagnosed it should be staged. This helps veterinarians determine how advanced the disease is and it allows them to better determine which treatments are most beneficial at this time. There are four stages of kidney disease with one being the least advanced and four being the most advanced. We also determine at this time if the pet has high blood pressure associated with the kidney disease, which may need to be managed. Finally, we determine if the kidneys are allowing larger protein molecules to be lost in the urine. If this protein loss is occuring it can dramatically change the treatment recommendations and overall prognosis.
Risk Factors and Causes of Kidney Disease
Usually once chronic kidney disease is diagnosed, there has been enough permanent damage to the nephrons that it can be very difficult to tell what actually caused the disease to begin with. In some cases, there was a known injury or insult to the kidneys weeks, months or years earlier that may be linked to the more permanent kidney disease. For example, if a dog accidentally ingests a large amount of ibuprofen (Advil) this drug has potential to cause a great deal of damage to the kidneys. Even if the pet is hospitalized and responds very well to treatment with kidney values in the bloodwork being normal at the end of the hospital stay, we know there may be some permanent changes that do not show up until much later. However, there are other pets that develop chronic kidney disease that have no known previous damage to the kidneys. Even with advanced testing, sometimes the cause is never found.
What we do know is that there are a few risk factors for developing kidney disease. There is still a lot of work that needs to be done in this area, but here are a few things that we know may be linked to kidney disease.
- Breed: There are certain breeds of dogs and cats that are more at risk for developing kidney disease. The specific types of disease may vary greatly amongst these animals. For example, Shar Peis are considered more at risk for developing kidney disease because they are more likely to create a protein called amyloid within the kidneys that causes permanent damage. While Persian cats are at risk of developing kidney disease because they form multiple cysts (fluid-filled sacs) within the kidneys. Some other dog breeds with a documented increased risk are Bull Terriers, English Cocker Spaniels, Cavalier King Charles Spaniels, West Highland White Terriers and Boxers. The cat breeds predisposed to kidney disease are Abyssinian, Siamese, Ragdoll, Burmese, Russian Blue and Maine Coon.
- Other Diseases: We do know there are some diseases that also put the kidneys at risk. How the kidney damage occurs varies greatly from one disease to the next, but here is a list of the diseases linked to kidney damage.
- Hypercalcemia (high calcium in the bloodstream)
- Heart Disease
- Dental Disease
- Cystitis (bladder inflammation)
- Bladder stones
- Hyperthyroidism (high thyroid hormone levels)
- Diabetes
- Certain types of infection (leishmaniosis, tick disease etc)
- Drugs: There are also several medications we know can cause some damage to the kidneys in certain patients. Often before a pet is started on one of the medications, the kidney values are assessed and monitored while the pet is taking these medications. Antibiotics like aminoglycosides or polymyxins as well as non-steroidal anti-inflammatories and certain chemotherapy agents all can place some extra pressure on the kidneys.
- Toxin: Because the kidneys are one of the major exit points for so many compounds entering the body they can be hit pretty hard when a pet ingests toxins. This is not an exhaustive list, but these are a few toxins known to cause significant kidney disease in dogs and cats:
- Lillies (cats)
- Antifreeze
- Grapes (dogs)

- Trauma: Direct trauma to the kidneys or major trauma to the entire body resulting in loss of blood flow to the kidneys can create permanent damage.
Treatment and Monitoring
The first critical step in managing chronic kidney disease is trying to find the underlying cause. This may require several different tests, including additional blood testing, urine cultures, ultrasounds and sometimes ultimately biopsy of the kidneys. Most pet parents work closely with the veterinarian to determine how far down this path of testing they would like to go. The veterinarian can help guide you based on history and other changes they are finding on exam/bloodwork whether or not they are suspicious of another underlying disease like hyperthyroidism, heart disease or bladder stones that may be contributing to the kidney disease. At minimum, most veterinarians like to make sure they are not missing something they could potentially treat and cure like a urinary tract infection.
By the time chronic kidney disease is diagnosed, most of the damage that has already occurred is permanent. Therefore, the treatment is mostly focused on slowing the progression of the disease and reducing the overall work load of the kidneys. Because the kidneys are such vital organs and have so many different jobs, this can become quite complex.
In the early stages, we can often accomplish most of what we want by simply modifying the diet to a prescription kidney diet. These work by restricting phosphorous, protein and sodium intake while also supplementing with polyunsaturated fat and potassium (for cats). There was actually a study that showed cats with chronic kidney disease fed a prescription kidney diet survived up to twice as long as their counterparts eating non-prescription diets.

As the disease advances, the veterinarian may want to keep a close eye on several different parameters that can change quickly. If they are noticing things fluctuating too much, there are many treatments they can intervene with to keep that happy balance within the body and keep your pet comfortable. Here are a few of the big things veterinarians like to monitor for patients with kidney disease.
- Hydration Status: This is a big one. Because the kidneys are so incredibly good at filtering they often can get rid of huge amounts of waste products while losing very little water. As the kidneys fail, a pet may begin to lose large amounts of water through the kidneys making it difficult to keep up with all of their body’s demands. In the early phases, a pet will drink more to compensate, which is why access to clean fresh water is so vital. However, as the disease advances, it becomes physically impossible for a pet to keep up with all of the losses and that’s when fluids need to be supplemented. In some cases, this requires hospitalization for a few days, but for maintenance, this is something most pet parents can accomplish in the home setting with a little training and guidance from their veterinarian.
- Nausea: The waste products that build-up in the blood stream when the kidneys are failing can cause some irritation to the stomach and nausea. They can also lead to painful oral lesions making it difficult to eat. Routine exams help the veterinarian know if oral lesions are forming and close monitoring by the pet parent helps us know if a cat or dog is losing their appetite or having vomiting episodes. Often, these things can be managed as long as they are caught.
- Blood pressure: Approximately 20%-30% of animals with kidney disease have high blood pressure as a result. The high blood pressure can cause many other concerning changes in the body, but can also make the kidney disease even worse.
- Phosphorous: It is common for phosphate to build up when the kidneys lose some of their filtering ability. This creates an imbalance in the calcium-phosphate
- Calcium: Much like with blood pressure, the relationship between calcium and kidney disease is cyclical. Kidney disease can cause high calcium levels in the blood, which can in turn cause worsening kidney disease creating a vicious cycle.
- Electrolytes: There is a delicate balance of electrolytes in the body which can have a variety of effects on everything from muscle contraction to blood pressure. The kidneys often help keep this perfect balance, and when they are not working well, these can easily become unbalanced.
- Protein Levels: Depending on the type of kidney disease, larger particles like proteins may be lost. If enough protein is lost from the blood stream, it can cause fluid build-up elsewhere in the body and potentially be life-threatening.
- Red Blood Cell Levels: In addition to being little filters, the kidneys also produce a hormone that tells the body to make more red blood cells. If the kidneys stop doing this part of their job, the red blood cell count can become dangerously low. The hormone (erythropoietin) can be supplemented for a time if needed.






Leave A Comment